Illinois House approves bill improving health insurance network adequacy standards
SPRINGFIELD, Ill. (WAND) — State representatives passed a plan Wednesday to improve network adequacy standards for health insurance companies.
The legislation could require insurance companies to notify patients of the anticipated date health care providers will leave their network and publish the information on their directories within 10 days. This plan also calls on insurers to provide contact information for patients to dispute inaccurate charges with a customer service representative.
Consumers would also have the ability to recoup their out-of-pocket payments if they were charged out of network costs for a provider listed in their insurance network. Insurance companies could be required to audit their health care provider directories every 90 days and make necessary corrections as well.
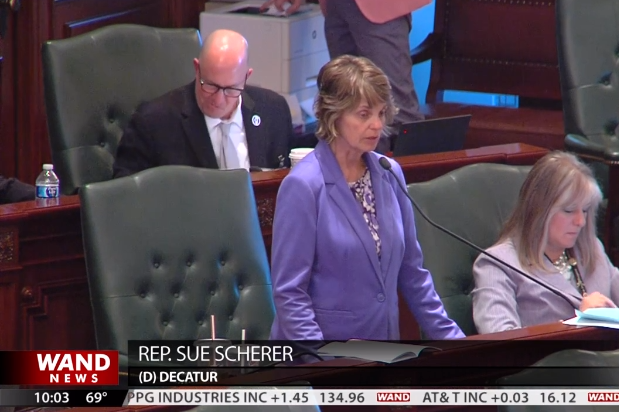
“It is a totally wrong practice,” stressed Rep. Sue Scherer (D-Decatur). “It is very unfair to the people who are paying their premiums in good faith thinking that they have a provider or doctor and then the doctor isn’t even there.”
